All of the following pertain to Neisseria meningitidis except: morphological characteristics, virulence factors, pathogenesis, epidemiology, prevention, and control. This bacterium is a Gram-negative diplococcus that causes a variety of diseases, including meningitis, septicemia, and pneumonia. Neisseria meningitidis is a major public health concern, and understanding its characteristics and behavior is crucial for effective prevention and control.
This comprehensive overview will delve into the distinct morphological features, key virulence factors, pathogenesis, global distribution, risk factors, serogroups, and strategies employed to combat Neisseria meningitidis infections. By exploring these aspects, we aim to enhance knowledge and contribute to the ongoing efforts to mitigate the impact of this significant pathogen.
Morphological Characteristics: All Of The Following Pertain To Neisseria Meningitidis Except
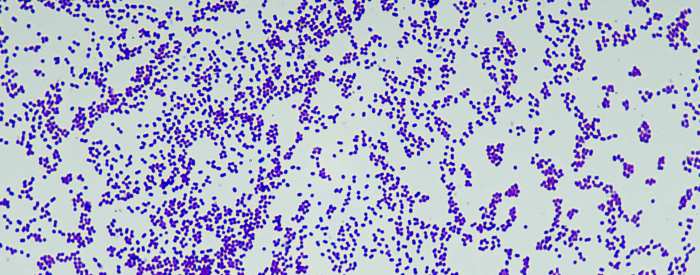
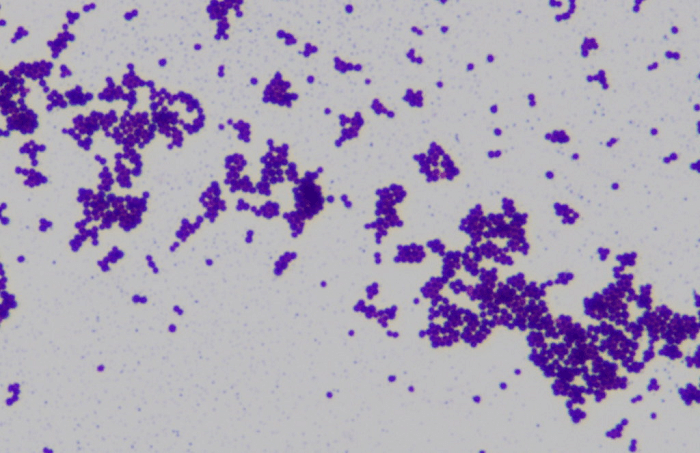
Neisseria meningitidis, a Gram-negative bacterium, exhibits distinctive morphological features that aid in its identification and differentiation from other bacteria.
The bacterium is characterized by:
- Shape:Diplococcoid, appearing as pairs of kidney-shaped cells.
- Arrangement:Diplococci arranged in pairs or short chains.
- Staining:Gram-negative, exhibiting pink coloration with Gram staining.
Virulence Factors
Neisseria meningitidis possesses several virulence factors that contribute to its ability to cause disease:
- Polysaccharide Capsule:Protects the bacterium from phagocytosis and immune recognition.
- Outer Membrane Proteins (OMPs):Facilitate adhesion to host cells and promote invasion.
- Lipooligosaccharide (LOS):Triggers inflammation and immune responses.
- Iron Acquisition Systems:Allow the bacterium to obtain iron, an essential nutrient for growth.
- Toxins:Damage host cells and contribute to tissue destruction.
Pathogenesis
Neisseria meningitidis typically colonizes the nasopharynx, and in some cases, it can invade the bloodstream and cause invasive meningococcal disease (IMD).
The pathogenesis of IMD involves:
- Nasopharyngeal Colonization:The bacterium attaches to the mucosal lining of the nasopharynx.
- Invasion:Through mechanisms such as OMPs, the bacterium crosses the mucosal barrier and enters the bloodstream.
- Bacteremia:The bacterium multiplies in the bloodstream, causing sepsis.
- Meningitis:The bacterium crosses the blood-brain barrier and enters the cerebrospinal fluid, causing inflammation and meningitis.
Epidemiology
Neisseria meningitidis has a global distribution, but its prevalence varies by region.
Risk factors for infection include:
- Age:Infants and young children are most susceptible.
- Geography:The “Meningitis Belt” in sub-Saharan Africa has the highest incidence rates.
- Immune Status:Immunosuppressed individuals are at increased risk.
Different serogroups of Neisseria meningitidis have distinct epidemiological patterns:
- Serogroup A:Common in the Meningitis Belt.
- Serogroup B:Most prevalent in Europe and North America.
- Serogroup C:Historically common in the UK, but now controlled by vaccination.
- Serogroup W:Emerging threat in many regions.
Prevention and Control
Prevention and control of Neisseria meningitidis infections rely on:
- Vaccination:Conjugate vaccines are effective in preventing infection by specific serogroups.
- Chemoprophylaxis:Antibiotics can be used to prevent infection in close contacts of cases.
- Public Health Measures:Early diagnosis, isolation of cases, and contact tracing help limit transmission.
FAQ Guide
What are the common symptoms of Neisseria meningitidis infection?
Common symptoms include fever, headache, stiff neck, nausea, vomiting, and sensitivity to light.
How is Neisseria meningitidis transmitted?
It is spread through close contact with respiratory droplets from an infected person, such as coughing or sneezing.
Who is at risk of Neisseria meningitidis infection?
Anyone can be infected, but certain groups are at higher risk, including young children, college students, and individuals with weakened immune systems.
How can Neisseria meningitidis infection be prevented?
Vaccination is the most effective way to prevent infection. Other preventive measures include avoiding close contact with infected individuals and practicing good hygiene.